The shocking killing of Jordan Neely has once again pulled the country’s attention towards our mental health-care system. The deadly act seems to me to be clearly criminal, but many others are already making the case for and against the prosecution of the man who killed him.
What I can’t stop thinking about is how Neely might possibly have been saved—and that leads me inevitably to the unpopular, permanently-controversial topic of involuntary commitment.
Neely’s troubled history has quickly become a matter of public record. It’s a tragic story: He spent years drifting into and out of psychiatric care, was well-known to city public health officials as a vulnerable individual, and frequently demonstrated instability and a tendency to sudden outbursts. Many have pointed out that the shocking murder of his mother in his adolescence profoundly destabilized him. Years of living an itinerant lifestyle, often without a reliable place to live, could only have contributed to his difficulties; use of dangerous substances like synthetic marijuana couldn’t have helped.
In many ways Neely was a quintessential example of a damaged person who fell through the cracks.
Neely appears to have been treated both voluntarily and involuntarily over the course of his life. It’s impossible to say whether he would have been saved by more compulsory care. But there’s a good chance that he could have been.
One of the most tragic elements of serious mental illness is anosognosia, a term which refers to the inability of the mentally ill to understand their own illness. Treatment-resistant patients, as Neely appears to have been, can be their own worst enemies thanks to this condition. Involuntary care can help get them medicated sufficiently to understand their condition, leading to the voluntary decision to stay in treatment.
It is, of course, a very serious step, to force someone into treatment against their stated desires, and it should never be done lightly. But for those barely holding on, such action can very well be the difference between life and death.
The current system, in most locales, makes it too difficult to force people into treatment when the alternative threatens their life. But to reform the system we need to understand where we are—now.
There’s a core element of this discussion that I wish I could teach every American: the world of mental health treatment described in the countercultural media of the 1960s and 1970s no longer exists.
Nurse Ratcheds are not prowling locked wards in ancient state-managed hospitals. I have found again and again that average people assume that the United States is filled with government-run mental health facilities and that all of us are just a bad day away from being sucked into one of them, unable to defend our rights or regain our freedom.
This is a strange misconception.
That countercultural tendency in the late 20th century I referred to, the idea that there is no such thing as mental illness—made famous in the wide-ranging and intense critiques of mental health care by Tomas Szasz, as well as by the book and Oscar-winning film One Flew Over the Cuckoo’s Nest, among many others—won that argument. Indeed, the changes to our mental health system that followed those efforts represent one of the biggest and most enduring victories achieved by those social movements.

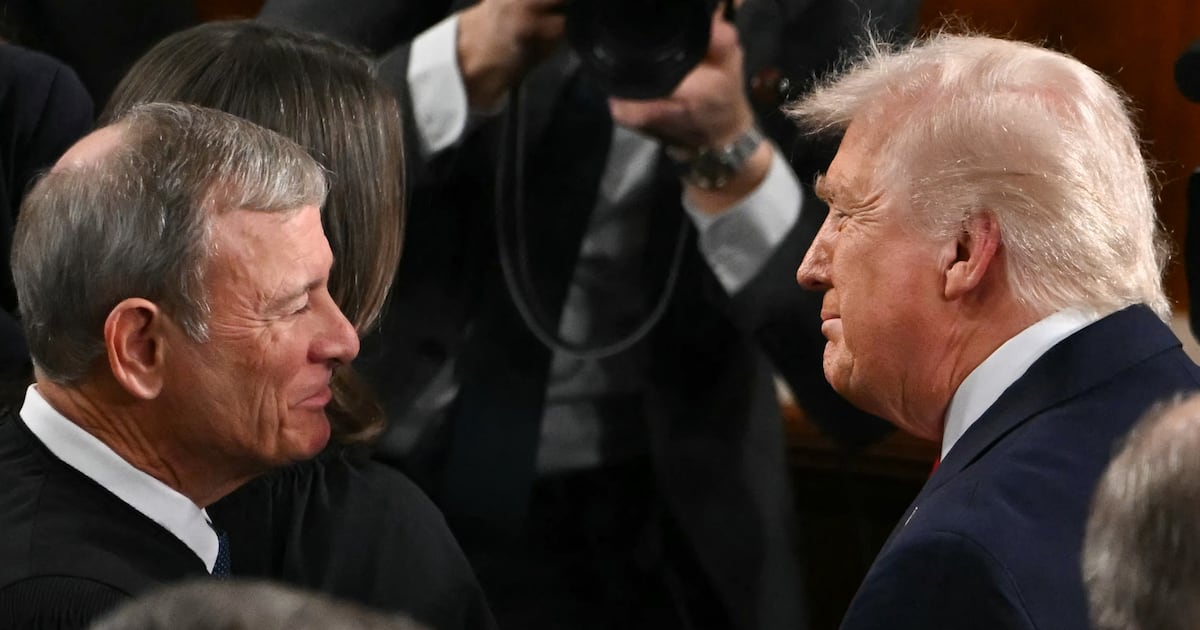
President John F. Kennedy signs into law the second phase of a two-part program to address the problems of mental illness in 1963.
Bettmann/Getty ImagesThe first major step to where we are now was deinstitutionalization. The last major piece of legislation that John F. Kennedy signed into law was the Community Mental Health Act of 1963. Arising from widespread claims that the asylums and psychiatric hospitals of the time were holding pens where patients faced awful conditions (claims that all too often were true) the law decreed that a large portion of those institutions would be closed, and in their place would be built a series of community mental health centers—perhaps as many as 1,500 of them, or so the plan went. The effort to close state facilities was successful, as dozens of psychiatric hospitals were closed following 1963. This was not a hard sell for state governments; indeed, deinstitutionalization offered them a perfect excuse to close expensive institutions and shift the cost burden of caring for patients elsewhere.
“Elsewhere” was conceived by proponents of the Community Mental Health Act as the previously mentioned community health centers, which would essentially act as a middle ground between inpatient and outpatient care.
Unfortunately, those community mental health centers were mostly never built. The amount of federal money earmarked for their creation was woefully inadequate. Worse, the law resulted in the kind of insufficiently-defined responsibility that allows both the federal and state governments to throw up their hands and say “Who, me?”
Ultimately, the states simply didn’t build the mental health infrastructure they were expected to, and the defining nightmare of deinstitutionalization was the outcome. Admittedly inadequate existing facilities were closed, nothing of remotely comparable size was built, and untold thousands of patients were forced to move in with family, or onto the streets, or into prison cells.
The introduction of Medicaid, an essential and lifesaving program, also created a perverse incentive where mental health care was concerned. As the American Medical Association’s Journal of Ethics describes, the particulars of Medicaid’s funding system “created an incentive for states to close the facilities they funded on their own and move patients into community hospitals and nursing homes partially paid for by Medicaid and the federal government.” Again, the states had an opportunity to cut spending which had been earmarked for a vulnerable population.
Meanwhile, most of the institutions that take Medicaid money are for-profit, and thus have the same fundamental mandate all for-profit entities do: to make money. This is a very different goal than treating patients effectively and humanely. And while I believe that general improvements to psychiatric care writ large make most of these institutions more humane than the old state hospitals, there’s no inherent reason why for-profit hospitals would be better than state facilities. And oversight over these places tends to be just as incomplete as everything else in our system.
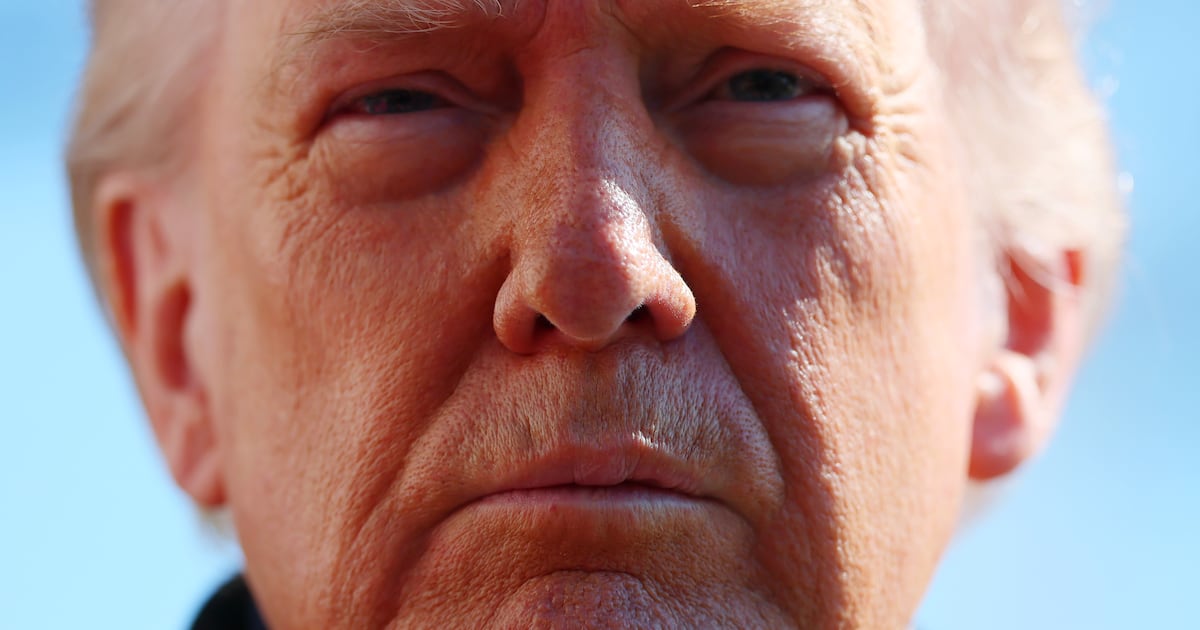
Core to the contemporary status of involuntary care is the 1975 Supreme Court case O’Connor v. Donaldson. It was that case that established the general standard under which involuntary commitment still operates: people with severe mental illness, even those actively psychotic or otherwise in crisis, should be involuntarily committed only if they represent an active danger to themselves or others. In practice, the implementation of involuntary care standards vary considerably between states, and practically, between individual hospitals. (So much depends on which doctor you catch.) Still, the general principle of involuntary commitment as a response to the potential for violent harm is a lodestone in American psychiatry.
To many, this sounds like a noble libertarian principle. In practice, it’s a nightmare.
Jonathan Rosen demonstrates the problems with this model in his indispensable new book, The Best Minds, about his childhood best friend Michael Laudor, a schizophrenic man who inspired many by graduating from Yale Law School and shocked more by murdering his girlfriend.
As Rosen shows, by changing the standard from treatment based on illness to treatment based on risk, the incentives of care were badly warped. Among other issues, a standard that insists that severe illness itself cannot be a reason for involuntary care cannot address the fact that those patients with a history of violence can often go from seeming calm to extreme violence very quickly.
The standard can also distort doctor behavior. One of the fundamental problems with American mental health care lies in the bifurcated inpatient-outpatient system. While the wealthy can always get discreet treatment in upscale hospitals that feature all the amenities of a resort, ordinary people have to confront equally unappealing alternatives.
The choice is often between immediate and uncomfortable inpatient care in facilities that deprive patients of autonomy and freedom, and which (contrary to many people’s assumptions) can leave you with huge medical debts. That route also often involves hunting for a doctor who will refer you and a facility with an open bed, which can be very daunting when in a psychiatric crisis. The other option is seeking outpatient care, which entails all of the difficulty of getting health insurance to pay for anything (if indeed you have insurance), with the additional problem that there’s a serious shortage of psychiatrists in this country, again while you’re suffering through a crisis. Contrary to what many people seem to think, every city does not have a hospital on the edge of town where you can just turn up and get help.
Now consider the way the standard of physical risk might complicate these issues. With that standard in place, doctors have every incentive to divide patients into two groups: those who are dangerous, and thus need involuntary treatment and are someone else’s problem, and those who aren’t, who can safely be pushed out into the street. ER psychiatrists are notorious for minimizing any problems that aren’t immediate, acute psychosis. This leaves patients in a crisis in the position of having to fight to be taken seriously by the very people who should be most sympathetic. As Rosen writes, with the standard of risk to self or others established, “a hospital would only produce a bed, or mandate treatment, for someone actively threatening harm.” This dynamic has hollowed out care and put both patients and doctors in an untenable position.
And in those cases where involuntary commitment really is inappropriate, it's likely often the product of doctors who fear the risk of a lawsuit. Were the standard of involuntary care based on the judgment of severity of illness rather than the potential for violence, doctors could navigate these issues on a case-by-case basis, without the cruel dichotomy of the current system.
After the development of case law, in the 1990s the Americans with Disabilities Act created additional pressure points that compel facilities to move patients out quickly, often more quickly than is medically appropriate.
The specifics of expansion to involuntary commitment statutes will ultimately be state-specific, but to be effective any such expansion must give social services workers more leeway to compel psychiatric evaluations, and doctors more leeway to hold patients.
The standard of violence as the single defining criterion of commitment, which has broken the experience of emergency room psychiatric medicine, must give way to a holistic appraisal of the degree of a patient’s impairment. Proposals to expand the state’s capacity to compel people into treatment float around frequently, but the concept remains deeply unpopular, in large measure because most people have no exposure to the system and no skin in the game.

Mayor Eric Adams arrives for a news conference at 1 Police Plaza in New York City on April 18, 2023.
Brendan McDermid/ReutersThe planned expansion in New York City has proven to be an albatross for Mayor Eric Adams, and media coverage has been almost universally negative. Similar plans have been discussed in Los Angeles, but they can be expected to meet the same headwinds. Resistance to involuntary commitment is easy for people who have never been confronted with true psychotic behavior, and the costs of not treating people—living on the street, dying of overdoses, being imprisoned for harming others, committing suicide—are conveniently out of sight.
Progressives emphasize that we need to provide more resources for the poor and marginalized to access voluntary care. It’s true, we do need more access, more ability to voluntarily receive care.
This means increases to Medicare and Medicaid funding, including getting the 10 states that have still not accepted the Obamacare Medicaid expansion to do so. It also requires muscular efforts to ensure that doctors and institutions accept these public health programs, given that they can often reject such patients out of hand, whether explicitly or through bureaucratic means.
Funding increases require raising taxes, particularly on the state level. Provider taxes, or taxes that fall on medical providers, would be an essential element of such revenue generation. On the federal level, the United States could join with essentially every other developed nation and pass a value-added tax, or VAT. It goes without saying that such increases would represent a major political lift.
Regardless, as I have tried to demonstrate here, our mental health crisis cannot be solved simply by expanding access, thanks to the treatment non-compliance of much of the mentally ill population.
Let me emphasize that point: Our mental health crisis is not merely a crisis of access; it is also a crisis of refusal.
I implore you to look at Jordan Neely and ask yourself if our current system is working and if more could have been done. The system that has for 60 years evolved to make involuntary commitment harder and harder could not save him.
It's currently failing the hundreds of thousands of people in this country who suffer from severe mental illness but go untreated, very many of them because they’re too sick to accept care. It’s failing the bystanders who face instability and rare but disturbing acts of violence that stem from our tattered system.
On the one hand, we have airy invocations of vague principles that sound good in speeches and rally donors for nonprofits. On the other, we have thousands of damaged people, dead from suicide or overdose, or living lives filled with pain. And I think it’s finally time to value the latter more than the former.