Yvon Guilavogui has four children living amidst an Ebola epidemic in his native Guinea.
And here he was in a New York City subway station on Friday morning, handing out one of the free morning newspapers.
“EBOLA IN NYC,” read the headline of AM New York.
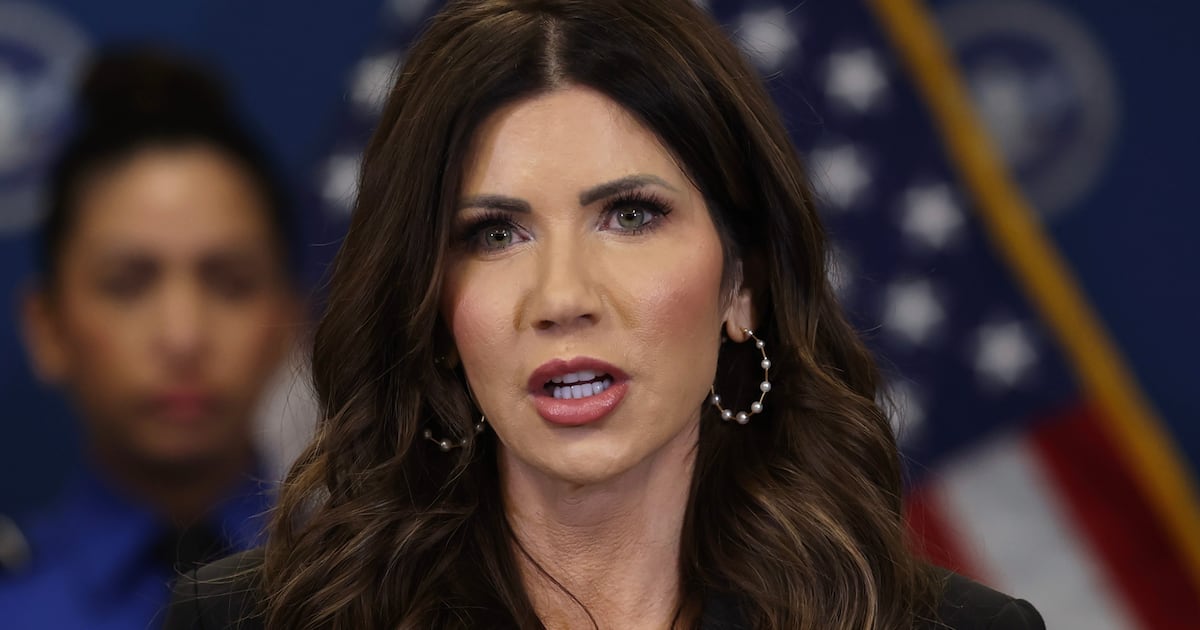
The front page carried a photo that 33-year-old Dr. Craig Spencer posted on his Facebook page in September of himself in the protective equipment he would wear as a volunteer in the fight against the virus in Guilavogui’s home country.
“Read about Ebola in New York! Don’t miss it!” Giulavogui cried, 55 years old and less than a decade in America, but sounding like a Gotham newsboy from another era.
He was holding up a paper as a woman approached with a child on her left hip, pushing an empty stroller with her right hand. She glanced at that word EBOLA and hesitated for just a heartbeat as she seemed to make a decision that appeared to be shared by all the others who trooped past.
They were all passing along what was widely known to be the very passageway that Spencer had taken on Wednesday evening from a downtown A train to a Brooklyn-bound L. But every one of these straphangers on Friday morning—including a number of mothers with strollers—seemed to have decided there was no reason to be afraid.
The vast majority of other New Yorkers had reached the same conclusion. The city may have learned something about resolve in the wake of the 9/11 attacks. But a good part of the reason for the present calm must be the seemingly flawless response by the emergency services and the medical people, beginning with Spencer himself.
Back when he was in West Africa, Spencer discussed the situation there with Dr. Les Roberts, who later wrote in his blog, “The primary health benefit of a patient going for treatment is not that they will get medical care and survive. The primary benefit is that they will not infect a slew of other people as they become viremic and shed via every pore and liquid in their body.”
Roberts added, “I can think of no other disease with the possible exception of rabies where the No. 1 health reason for medical care is not related to the patient.”
Spencer had returned from Guinea on Oct. 17, saying he was confident his protective gear had kept him from becoming infected. He had still not been experiencing any symptoms to tell him otherwise on Wednesday, as he hopped the subway to bowl in Williamsburg.
Around 11 a.m. Thursday, Spencer determined that he had developed a fever of 100.3. He immediately contacted the humanitarian organization that he had worked with in Guinea, Doctors Without Borders, also known as Medecins Sans Frontieres, or MSF. The organization contacted the FDNY, whose Emergency Medical Service dispatched a specially equipped HAZ TAC ambulance to his apartment in West Harlem at 11:52 a.m.
Recently, emergency operators in New York have begun asking callers if they had been in West Africa in the previous 21 days and if they were running a temperature. Some three dozen had answered affirmatively to both and were deemed “fever with travel” jobs. None of them had tested positive for Ebola.
But this patient was a doctor who had been treating people with Ebola in a facility awash with hyper-infective fluids. The HAZ TAC paramedics donned special protective gear before they ventured inside the building. They would have only praise for Spencer.
“This guy’s in pretty good shape, very cooperative, very understanding of the process,” an EMS official later said.
Spencer even thought to lock his key in the apartment lest somebody end up taking it and use it to gain entry before the place was decontaminated. The ambulance sped off in the rain with a police escort, across the top of Manhattan, then down along the East River and into an isolation entrance that had been established at Bellevue Hospital. Everything proceeded with a smoothness and precision born of training drills.
“Textbook,” the EMS official said.
Two hours after he first noted his symptoms, Spencer was in an isolation unit that had been established years before, when another African virus, HIV, first struck the city. He was attended by a medical staff wearing much the same protective gear he had worn treating Ebola patients in Guinea.
“The first thing on the list of care was to draw blood,” the EMT official said.
The blood was rushed to the NYC Public Health Laboratory, the oldest such facility in the country, established in 1892 to combat endemic diphtheria. The lab conducts more than 2 million tests on more than 400,000 specimens a year. Few, if any were ever awaited with greater public interest than this one.
In West Africa at the present, an Ebola test can take four days or more and that is if the sample is not lost. The test here in New York took four hours.
The result was positive, which meant that at least one particle of virus had infected Spencer in Guinea and proceeded to replicate as he flew to Belgium and then on to New York. He now gave the NYC Health Department’s medical detectives a list of everyone he had been in contact with since he had become symptomatic; two friends as well as his fiancée, who was immediately quarantined. He handed over his fare card so detectives could determine exactly when he had entered the subway system. He made only one unrealistic request as he sought to keep others from becoming infected and began a fight for his life.
“He said he didn’t want any media on this,” the EMS official said.
His name quickly leaked out and that picture he had posted on his Facebook page for his friends to see had now been displayed by seemingly every media outlet. That included the morning newspapers, but Guilavogui did not let the headline keep him from disturbing his usual good cheer along with copies of AM New York.
“Good morning,” he said again and again, sometimes adding, “Have a nice weekend,” at least once receiving a, “You, too.”
A homeless man paused and seemed only to see the emblazoned word “EBOLA.”
“Don’t scare the people,” he said.
“It’s not me,” Guilavogui replied.
The people seemed not at all frightened as they trooped past to begin their day. Guilavogui allowed that there was reason to be afraid back in his native land.
“I’m trying for my kids to come,” he said. “Three girls, one boy… 18, 15, 10, 7.”
He telephones his kids every day in his hometown of Macenta, which happens to be the second locale where the present Ebola outbreak struck. He gives them daily reminders to be careful and to keep a bowl of water mixed with Clorox by the door.
“When you go out, clean your hands, when you come back clean your hands so to be safe,” he told The Daily Beast. “That’s the only help you can get. They say there is no medicine.”
The residents of Macenta were initially so panicked that some stoned a team from MSF in the unreasoning fear that these foreigners might have brought the contagion they were actually fighting to contain.
MSF briefly withdrew, but then returned and proved able to bring the virus under control using the same principles of education and quarantine and contact-tracing presently employed in New York and elsewhere. But word that the Macenta area was relatively safe drew people from danger zones. Some brought Ebola with them.
The epidemic was flaring anew last month, when Spencer left New York for Guinea. He placed himself at risk not just for the sake of people in Guinea such as the Guilavogui kids, but for people back in America as well, along with any place else Ebola might possibly travel, which is just about everywhere.
Spencer is kin in spirit to soldiers in World War II who fought in Europe and the Pacific so we did not have to fight here and who sought to save all humanity from a great evil. He truly is a doctor without borders, even said to speak seven languages.
Some twits have gone on Twitter to suggest Spencer was being reckless when he went out bowling. The fact is that he had not yet developed a fever and he posed virtually no threat as he embarked on night out—well-earned after witnessing so much death and suffering in Guinea, risking the same fate while seeking to keep us all safer.
Everyone who took a paper from Guilavogui was taking a front-page photo of a médecin avec courage, someone who deserves our profound admiration and deepest hopes for a full recovery.
Spencer was listed in stable condition up at the hospital as Guilavogui handed out the last copy. Guilavogui clapped his empty hands together and went up to the street to fold the newspaper dispensers up by the subway entrance.
Just down West 14th Street was the Redden funeral home, the only one that would handle AIDS cases at the start of that epidemic in New York. The city is calm now, but that could change if Spencer’s colleagues lose the desperate fight in West Africa and we get more and more cases here.
The subway could suddenly not seem so risk-free. The counterterrorism checkpoints periodically set up by turnstiles could check temperatures as well as backpacks.
At day’s end, Guilavogui returned to his home away from home in upper Manhattan just seven blocks from where Spencer resides. Guilavogui made his daily call to his children and later was able to report what he hopes he can continue to say thanks to the efforts of all those médecins avec courage.
“They’re fine,” he said.
The next newspaper he would hand out in the subway would carry a report that the powers that be in New York state and New Jersey had been more alarmed than had many of the city’s residents. There would henceforth be a mandatory 21-day quarantine only all people arriving at JFK and Newark airports who had direct contact with Ebola victims in West Africa.
We should all hope that this does not dissuade other doctors such as Spencer from setting off to do what must be done for all our sake.