As states around the U.S. scavenge for ventilators to treat the wave of critically ill coronavirus patients, doctors on the front lines are confronting not just the question of when they will get them, but when they should use them.
The grim fact is that most people infected with COVID-19 who are sedated, intubated, and hooked up to a mechanical breathing machine will not survive. This is in part a function of just how sick they are when doctors finally resort to a ventilator, but also due in part to the damage ventilators cause to the lungs. The longer someone is on a ventilator, the lower the odds they will ever breathe again on their own.
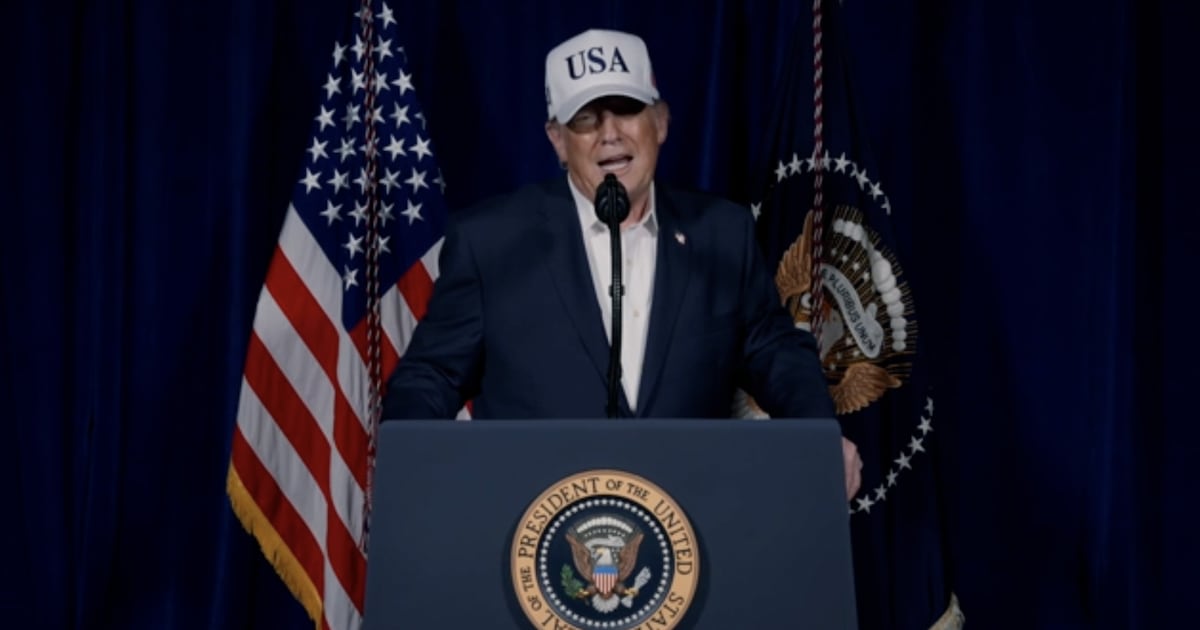
“It’s just a bridge to keep them going,” Marco Garrone, an emergency-medicine physician in Turin, Italy, told The Daily Beast. “It’s just a sort of last-ditch resort to buy time for them to heal... for the whole body to overcome the illness.”
But unlike with some other respiratory diseases, there is no proven treatment for COVID-19. Doctors around the globe have reported survival numbers that show how difficult it is for an intubated patient to outrace the disease. Garrone and his colleagues say only 20 percent make it, while a London study found a slightly larger proportion.
“These patients do extremely badly on mechanical vents,” Garrone said. At the same time, ventilators also represent the only hope for those whose oxygen levels continue to plunge—explaining why U.S. governors are so desperate to make sure they have enough.
“You need ventilators, that’s for sure,” Garrone emphasized. “I agree 100 percent with what Gov. Cuomo said.”
The challenge then is to find something less extreme than a ventilator to act as the bridge and buy patients the time they need to recover—a challenge that is all the more daunting given that doctors and researchers are still learning how the novel coronavirus behaves.
“It is a brand-new disease,” Derek Angus, of the University of Pittsburgh Medical Center and a renowned authority on intensive care, told The Daily Beast.
Before moving to a ventilator, Garrone often uses a mask to administer oxygen via continuous positive airway pressure, or CPAP. He compared it to home CPAP machines used to keep open the airways of people with sleep apnea.
“Exactly the same,” Garrone said. “Higher pressure.”
He added, “I have a good number of people who did really well on CPAP. I’m not saying everybody fares well, [that] CPAP works with everyone. Start them on CPAP and try to keep them on CPAP as much as you can.”
Another non-invasive option is a high-flow nasal cannula (HFNC), which delivers oxygen via a two-pronged tube fitted to the nose rather than via a mask as with CPAP.
But both methods can potentially aerosolize virus particles, sending them into the air. That is not a threat to COVID-19 patients, but could constitute a considerable danger to those not infected with the disease, including health-care workers and first responders—especially those running short of personal protective equipment.
In Kirkland, Washington, county health officials postulated that paramedics may have inadvertently furthered the spread of coronavirus when they employed CPAP machines to treat residents of the Life Care Center nursing home—where dozens eventually died.
Angus said on a Journal of the American Medical Association (JAMA) podcast last week that the jury is still out on whether the high-flow nasal cannula could pose a similar problem.
“We have not worked out at this point exactly how safe that is,” he said.
Further complicating the question of when to intubate is the deceptive and mercurial nature of COVID-19. A bad turn can come just as quickly as a new one.
Greg Neyman, an emergency physician in New Jersey, has noted that COVID-19 patients can appear to be in little distress at oxygen levels that ordinarily would have people gasping for breath and maybe tearing off their air mask. Instead, COVID-19 patients can appear to be “just a little fluish.”
“It’s something we’re not used to in emergency medicine and critical care,” Neyman told The Daily Beast.
The coronavirus patient’s lungs continue to function mechanically. But even as they inhale and exhale, inflating and deflating their lungs, they can be hypoxic, or short of oxygen in the blood. The lungs may work, but the oxygen does not reach them.
And there is a concern that an exhausted and overwhelmed medical staff might fail to note ongoing labored breathing.
“How safely can we use non-invasive ventilation?” Angus asked the JAMA podcast. “It would be terrible if [a patient] had acute respiratory failure without someone able to get to the bedside and intubate.”
Because COVID-19 can worsen so precipitously, doctors may have only a small window in which to make the decision to intubate.
When the time comes, Garrone asks the patient—who is generally still conscious and cognizant—for verbal consent before inducing a coma from which they have a painfully low chance of emerging.
“I don’t think they are aware of how the odds are against them and it would be very harsh of us, almost cruel, to tell them,” Garrone told The Daily Beast. “Besides, when they are proposed with intubation there is really no other reasonable course of action left.”
Doctors are trying to figure out new courses of action in real time, as their ICUs fill up and their ventilator supplies run low. Researchers are racing to analyze the outcomes to better inform the decision-making process.
“We don’t know enough yet,” said Angus. “We want more data.”
He offered a comparison of the fight we face with brand new COVID-19.
“Trench warfare in the First World War,” he said.
But in truth, the life-and-death decisions on the battlefield were simple compared to those faced by ICU doctors. Even when hospitals have enough ventilators.