The COVID-19 pandemic has made the pulse oximeter something of a household item, for at least a large chunk of the public. The devices, which measure a person’s pulse and the amount of oxygen carried in their blood, inform a common benchmark for managing COVID infections: If someone’s oximeter reading indicates a 92 percent oxygen saturation or lower, they need to go to the hospital immediately.
Clinicians rely on pulse oximetry as a basic vital sign, not just for COVID. Concealed within “normal” blood oxygen measurements above 92 percent, however, are cases where a pulse oximeter’s estimate of blood oxygen levels are erroneously high. In a new study published Wednesday in the journal BMJ, researchers found that pulse oximeters failed to detect hypoxemia (i.e., oxygen deficiency) in Black patients at a rate 1.25 times higher than in white patients.
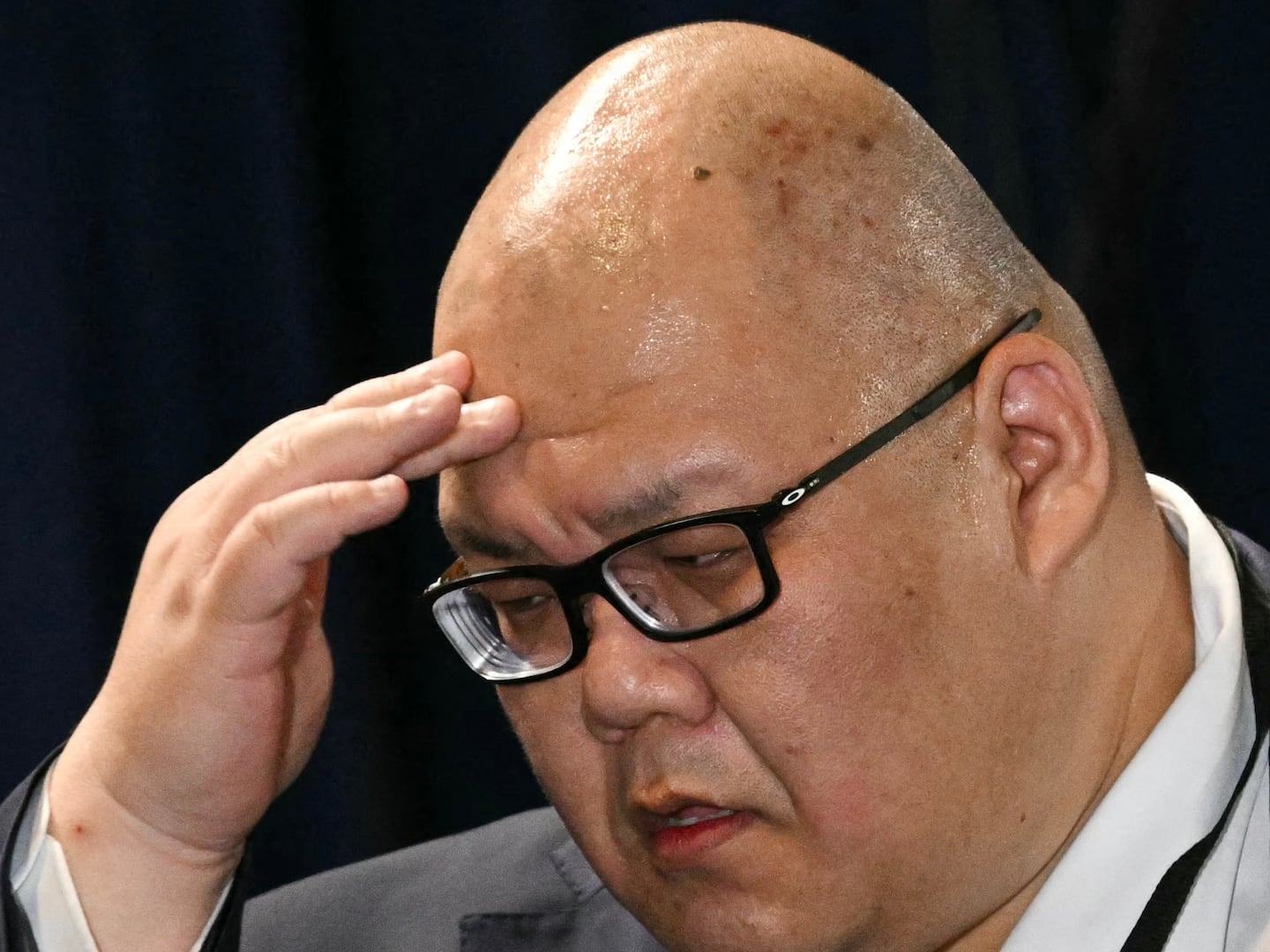
The reason is infuriatingly simple, study lead author Valeria Valbuena, a general surgery resident at Michigan Medicine, told The Daily Beast. Pulse oximeters made today rely on two wavelengths of light to measure blood oxygen levels, and melanin is one factor that affects the accuracy of their readout. In other words—these devices haven’t been designed for accurate use on people with darker skin.
“There has been information about this for as long as I have been alive, and I didn't learn any of this in medical school or residency,” Valbuena said. “It drives me insane.”
Valbuena took pulse oximeter readings at face value while treating patients for COVID at the beginning of the pandemic. But she soon noticed that Black and darker-skinned patients with pulse oximetry readings in the range considered “normal” were doing worse than white patients. She and her colleagues realized that the culprit was the oximeter, and they published a letter in the New England Journal of Medicine in December 2020.
Still, it was not known how large the scale of this problem was, since research on racial bias of pulse oximeters has largely focused on a subset of patients with severe illness. For the new BMJ study, Valbuena and her colleagues analyzed pulse oximeter readings and arterial blood gas readings (a measure of blood oxygen that requires a needle) from hundreds of thousands of hospitalized patients receiving non-intensive care from the U.S. Veterans Health Administration from 2013 to 2019. They found that hypoxemia not caught by pulse oximeters occurred in 15.6 percent of white patients but 19.6 percent of Black patients—a result in line with other estimates.
In fact, this disparity means that instances of hypoxemia must have been missed among the study’s own subjects. According to the research, over half a million additional instances of oxygen deficiency “would have been detected if pulse oximeters performed as well in [B]lack patients as in white patients.”
The team also found that white patients whose pulse oximetry estimates matched up with arterial blood gas readings were likely to have agreeing readings for the two methods at a later time, while this was less likely for Black patients.
A maddeningly simple solution exists for these biased measurements: Use better oximeters. And they exist! Equitable oximeters that incorporated more wavelengths of light to reduce skin-tone bias were designed in the 1970s. But instead, the two-wavelength models took off and now dominate the market. In June, the Food and Drug Administration announced that it will convene a public meeting to discuss concerns about pulse oximeters’ reduced accuracy among people with darker skin.
Valbuena hopes the results of this study will guide better treatment decisions for Black and darker-skinned patients. She recommended that patients with darker skin put more faith in their symptoms than in a “normal” pulse oximetry reading; clinicians, herself included, should rely on repeated arterial blood gas measurements, even though the technique is more invasive and painful.
She said that she tells her patients: “I'm subjecting you to more of this invasive test, because I can’t trust the machine that I have right now to keep you safe.”