Scouted selects products independently. If you purchase something from our posts, we may earn a small commission.
Walk into any upscale med spa these days, and you’re likely to encounter the beauty industry’s latest obsession: exosomes. These microscopic cellular messengers are being touted as the next big thing in hair restoration, promising to reverse thinning locks without the side effects of traditional treatments like minoxidil. But beneath the glossy marketing claims lies a more complex reality, one where legitimate science mingles with regulatory gaps and (some) unsubstantiated hype.
“Right now there’s a lot of hype, with various companies jumping on the bandwagon to make a quick buck, but there’s also a growing body of research,” says Dr. Jessica Wu, a Beverly Hills dermatologist, author, and authority on regenerative medicine, who offers exosome treatments in her practice. The question facing consumers: How do you separate science from snake oil?
What Are Exosomes?
“Exosomes are tiny vesicles (packets of biological substances) naturally secreted by cells,” Wu explains. “They deliver instructions to cells to help repair and promote regeneration.” Think of them as cellular mail carriers, transporting proteins, lipids, and other biological information between cells throughout your body.
This cargo can vary dramatically depending on the source. The most studied exosomes for regenerative medicine come from mesenchymal stem cells, often derived from umbilical cord tissue. But they can also be sourced from human fat cells, platelets, or even plants, a diversity that raises important questions about standardization and effectiveness.

The Science Behind the Claims
Unlike their predecessors in regenerative medicine, exosomes offer some theoretical advantages over treatments like platelet-rich plasma (PRP). “Unlike stem cells, exosomes are not living cells,” Wu notes. “They come from stem cells, but they can be purified and standardized, making them easier to use than stem cells.”
Wu, who briefly offered PRP treatments, found them lacking. “Many of my patients saw limited improvement. PRP is unpredictable; it depends on the patient’s blood quality. By contrast, exosomes are more reliable and potent, if sourced and stored properly.”
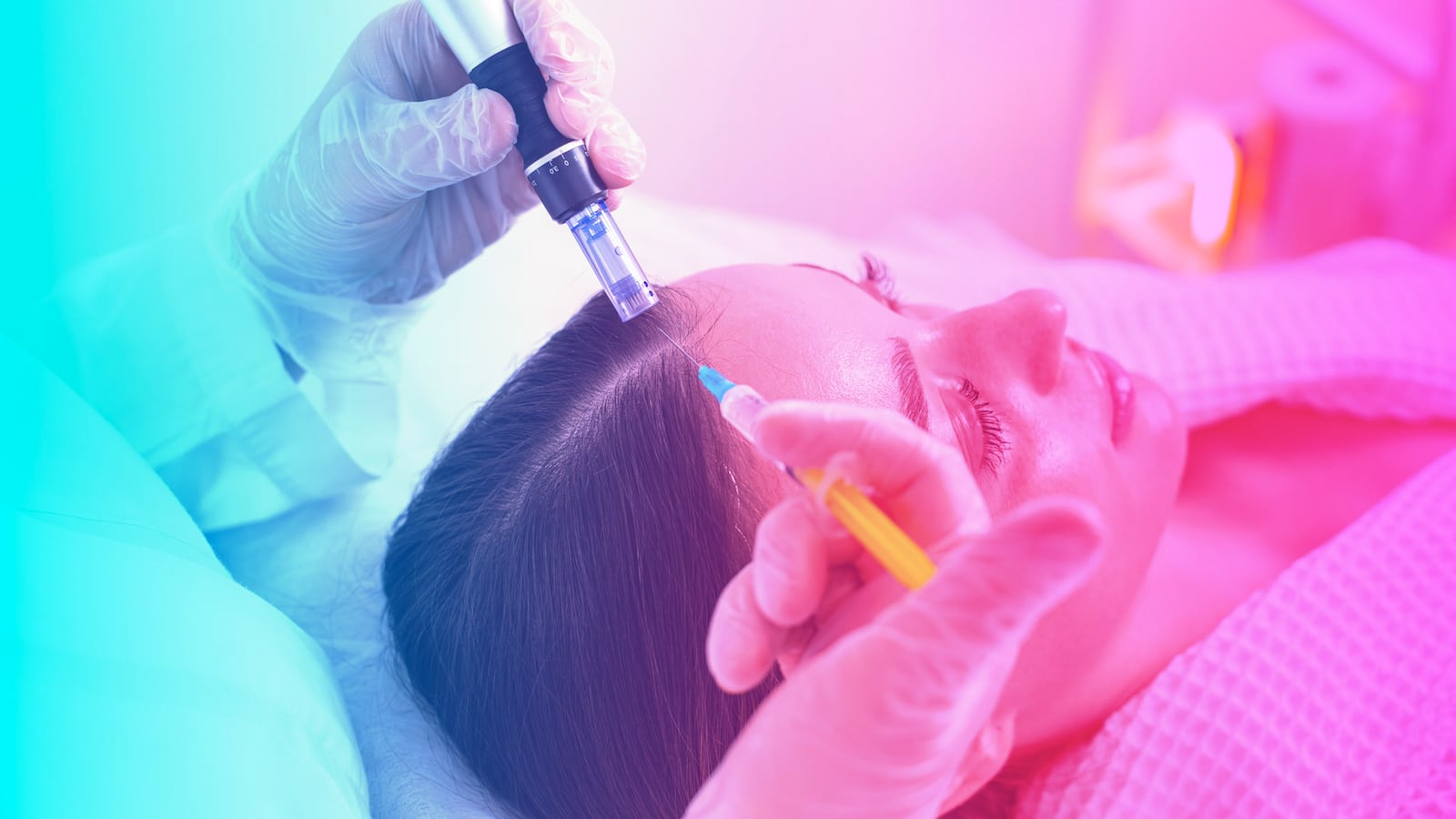
Early research suggests the delivery method matters significantly. Exosomes can be applied topically, micron-needled into the skin, or injected directly into the scalp. Wu reports that injection appears most effective because “the scalp is thick, and it’s hard to get ingredients to penetrate.”
The treatment seems particularly promising for androgenetic alopecia, the most common form of hair loss. “Androgenetic alopecia is the most commonly treated, most responsive, and most studied type of hair loss treated with exosomes,” Wu explains. She’s also seen success in patients recovering from telogen effluvium, the temporary shedding that occurs after illness or stress.
In limited head-to-head studies, exosomes have shown promise against PRP, with injected exosomes outperforming PRP in terms of visible regrowth. However, comparative data with established treatments like minoxidil or finasteride remains scarce.

The Timeline and Reality Check
Patients considering exosome therapy should set realistic expectations. Wu reports that many patients notice reduced shedding within four to six weeks, but visible thickness takes longer. “It takes three to six months for the hair to grow long enough to notice thicker, fuller hair on their heads,” she says.
The treatment isn’t a one-and-done solution either. Wu typically recommends maintenance treatments every few months once patients achieve their desired results, though long-term data on durability remains limited.

Red Flags for Consumers
Here’s where things get concerning. “Exosomes are the Wild West in skincare, because there’s currently a lack of regulations over how they are derived and processed,” states Dr. Joshua Zeichner, director of cosmetic and clinical research in dermatology at Mount Sinai Hospital in New York City. This regulatory vacuum has created a marketplace where quality varies dramatically between providers.
The risks aren’t just theoretical. Wu has seen “reports of infections and scalp inflammation due to improperly handled or contaminated products.” Even more troubling is Zeichner’s observation that “if there is genetic material like DNA or RNA in the exosome, there is a theoretical risk of transferring genetic material or even a disease to another person.”
Both experts emphasize the importance of due diligence when considering exosome treatments. Wu recommends asking pointed questions: Where do the exosomes come from? How are they stored? They should be refrigerated. The over-the-counter market is particularly problematic. “Exosomes are fragile and must be stored cold,” Wu explains. Who is performing the treatment—a physician or a technician? Will there be a medical evaluation to determine the underlying cause of hair loss?
“I’ve seen patients spend thousands with no results, only to discover later that they had an underlying medical condition,” Wu notes. In her practice, she’s identified thyroid disorders, iron deficiency, PCOS, and even toxicities in patients who initially sought treatment for hair thinning.

Making the Right Choice
For patients considering exosome therapy, the experts recommend starting with a comprehensive medical evaluation. Zeichner advocates for a multi-pronged approach: “Whether or not you’re getting exosome treatments, I still recommend vitamin supplements, red light treatments, and prescription medication like oral minoxidil.”
Wu agrees, noting that in her practice, “the first step is always a comprehensive evaluation. I examine the scalp and hair quality; take a full health and medication history; often draw bloodwork in the office; discuss hair care, styling, and topicals; and identify any underlying medical or hormonal issues.”

The Bottom Line
Exosome therapy for hair loss sits at the intersection of promising science and regulatory uncertainty. While early research suggests potential benefits, particularly for androgenetic alopecia, consumers must navigate a marketplace filled with unsubstantiated claims and variable quality products.
“I believe exosomes will be a cornerstone of regenerative dermatology for both scalp and skin,” Wu predicts. “We’re just scratching the surface of what can be achieved.” But she’s quick to add that rigorous, ethical studies are needed to determine optimal protocols and identify the best candidates for treatment.
Until then, caveat emptor remains the wisest approach. If you’re considering exosome therapy, seek treatment from a qualified physician who will conduct a thorough medical evaluation first. Ask tough questions about sourcing and safety. And remember that while the science is promising, we’re still in the early chapters of understanding how these cellular messengers might revolutionize hair restoration.
In a field where hope often outpaces evidence, a healthy dose of skepticism (paired with expert medical guidance) remains your best protection against both empty promises and genuine medical risks.