As major cultural events are forgotten, workplaces, bars, and restaurants close, and prominent politicians around the world have been sickened, two simple questions about the novel coronavirus pandemic seem to rise above the rest: How long will this last? And how will it end?
William Haseltine, president of the global health think tank ACCESS Health International, who recently chaired the U.S.-China Health Summit in Wuhan, where the virus likely originated, has a theory.
“There are four ways,” the doctor told The Daily Beast. “One, it peters out with the weather. Two, everybody gets infected, so it’s got no new places to go... so it ends—but that’s a pretty horrible ending. Three is a vaccine, which is about a year away. Fourth way is the most likely: We’re going to have a few drugs, within a few weeks to a few months, that prevent people from getting infected—like PrEP for HIV—and for treatment.”
Let’s break those down.
“There are four coronaviruses which cause upper-respiratory infections like the common cold,” said Arnold Monto, a professor of epidemiology and global health at the University of Michigan who has advised both the World Health Organization and the Defense Department on communicable diseases. “Those tend to be very seasonal.”
But there’s no guarantee that will happen with this new, deadly 2019 novel coronavirus, he added: “There’s so much unknown.”
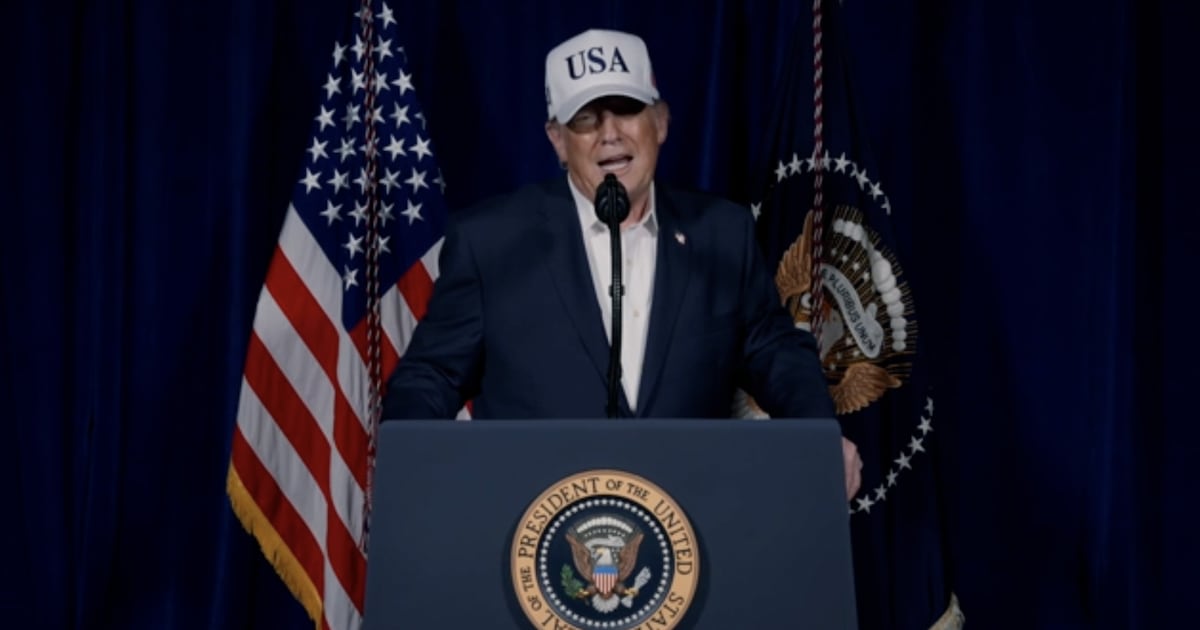
President Trump has been widely mocked for framing the outbreak, at least early on, as a problem that would disappear when the snow melts. But he wasn’t entirely off-base, experts have said.
Based on the epidemiological evidence currently available, there’s reason to believe that “with warmer, more humid weather” the virus will spread less efficiently, leading to a drop in cases, said Jeffrey Klausner, an adjunct professor of epidemiology at the University of California Los Angeles who previously worked for the Centers for Disease Control and Prevention.
“With a reduction in cases, anxiety and panic will go down,” he added. “Severe illness will decrease, and we can go back to business as usual.”
Even the deadly hotspot in, for example, New York, would eventually cool, allowing museums and Broadway productions to reopen for the masses.
Unfortunately, that’s just one possibility.
The pandemic could spread consistently through the summer—unmitigated by a vaccine or therapeutic treatment—until everyone who can get the virus does get it, until there’s no one left to infect, in what Monto called “the worst-case scenario.”
“I cannot get my head around 40 to 70 percent of the population being infected within the next few months, with a 2 percent fatality rate,” said Monto, painting a picture of a world where millions of Americans die and hundreds of millions of Americans might become infected.
In that situation, of course, nearly every aspect of life—business, education, cultural activity, agriculture, productivity, mental health—would be hit by likely irreparable damage. Without public gatherings, and at those numbers, it might be hard to even conduct funerals. As of Thursday, there were more than 451,491 cases in the United States, and New York City alone had surpassed 5,000 deaths.
Instead of imagining that future, said Monto: “I have chosen to believe that we are going to be able to control this by non-pharmaceutical interventions.”
But, as Klausner reiterated, once the infection spreads widely enough, “there’s no more people to become infected.”
“That is contributing to the declines we’ve seen in China and in South Korea and in Japan,” he explained. “People in these highly localized areas, because of the broader spread of infection, have developed immunity.”
But until that happens to everyone everywhere, “the virus can still travel across the globe to naive communities, cause outbreaks, and then go away,” said Klausner.
In another scenario, things could continue to spread and get worse until someone develops a vaccine. But that’s at least one year away.
Anthony Fauci, director of National Institute of Allergy and Infectious Disease, has said that a potential vaccine will enter a Phase One clinical trial in April, and—if it proves to be effective—could find its way to the public within 12 to 18 months. Other potential vaccines are in the works in the U.S. and elsewhere, but none are likely to hit shelves any sooner, Fauci has said.
On the bright side, both Haseltine and Klausner said there’s reason to believe therapeutic treatments may be available to the American public within just a few months.
When SARS and MERS came along, Haseltine explained, “there was a huge effort to create drugs,” many of which were promising leads. But then those two outbreaks, which both had significantly higher fatality rates than the novel coronavirus, petered out. Amid the new pandemic, physicians have picked back up on those prospects and begun to test them more aggressively.
Haseltine said the likelihood is that at least one treatment option will be available through the public-health system within weeks or months, and might even prevent the virus.
Klausner named two specific medicines that look promising, including remdesivir and actemra, the latter of which he called “essentially a synthetic antibody” that is “currently being used and recommended for use in China” to treat the new coronavirus. It has been jointly manufactured by Roche and Chugai Pharmaceutical for use as an anti-inflammatory drug for rheumatoid arthritis.
Meanwhile, remdesivir, which was created by Gilead Sciences, has been reported as the most promising possible treatment for the virus because it is a “broad spectrum” drug that has shown effectiveness against various viral targets in lab testing.
Officials expect outcome data on remdesivir as early as April, and there have been promising studies in cell culture and animal models, according to Klausner. “People are using the drug now in the United States under compassionate use,” he said, referring to an agreement between the manufacturer and the Food and Drug Administration that makes it available for some high-risk infected individuals. “It’s being used internationally as well.”
“Once the data are available and presented to the FDA, I would expect that FDA approval would be within a few days to a couple of weeks,” followed by a public rollout, said Klausner, who explained that there are multiple ways to use antiviral drugs, including prevention and treatment.
“For the flu, we use [antivirals] for treatment and prevention and prophylaxis,” he added. “In a setting where there’s an outbreak, we distribute the drug to people who may have been exposed.”
Unlike the way PrEP involves widely distributing anti-HIV medications to keep negative individuals from becoming infected, antivirals for respiratory diseases would likely be used strategically in hotspots with defined clusters of outbreaks involving at-risk populations, like in nursing homes and exposed families.
Though Monto said he disagreed with Haseltine and Klausner’s optimistic timelines for available therapeutic treatments, he still thinks Americans are not headed for the worst-case scenario.
Americans, he said, will likely see further outbreak—and then case decline—similar to how the SARS epidemic spread in 2002 and 2003: “The scenario, therefore, is: We will have hotspots, it will persist for one or two months, and then it may go away, and we may never know why.”
In the meantime, according to Monto, the world will look much like it does now, with local and federal authorities employing non-pharmaceutical techniques like (increasingly aggressive) social-distancing.
“We may see generalized transmission at a low level,” because no place is immune, but the majority of cases, Monto added, will likely be clusters that can be traced to one—or even a few—super-spreaders.
A super-spreader is a relatively rare epidemiological phenomenon, also present in SARS, where some carriers of the coronavirus are much more contagious than the average patient. Experts have pointed to possible super-spreaders of the virus as the root of clusters in the U.K., on the Diamond Princess cruise ship in Japan, and even in Chicago.
“We don’t really understand how this virus transmits differently in different places, but this virus has super-spreaders,” said Monto, pointing to the New Rochelle, New York, case of a lawyer who was infected, then ostensibly transmitted the virus to his wife, children, several neighbors, and even his rabbi. Just days later, more than 100 people in Westchester County, about 20 miles north of New York City, had confirmed cases of the virus, leading Gov. Andrew Cuomo to create a one-mile containment zone around the city, with help from the National Guard.
“The New York case sounds like a super-spreader,” said Monto. The city has since closed its public schools, broadway, movie theaters, bars, and restaurants—except for takeout—and there have been similar shutdowns across most of the country.
Shortly afterward, the CDC issued new national guidance suggesting the cancellation or postponements of any events involving more than 50 people anywhere in the U.S.
The CDC said in February that it planned to implement surveillance testing—in which hundreds of people in potential hotspots like New York and Los Angeles are tested to proactively measure the virus’ presence. ProPublica reported that epidemiologists in countries all over the world have heavily relied upon this sort of testing in order to track the spread of the disease before, instead of after, large numbers of patients end up at hospitals.
But systemic problems in rolling out effective tests quickly enough have plagued the American response to the outbreak, and slowed authorities down by weeks. The lack of tests has led to a distrust in public numbers and an inability to track the spread of the outbreak as it has ravaged the country.
Haseltine called the “the unavailability of test kits in the United States” a “serious failure of government,” noting that authorities “had two-and-a-half months of warning before we really needed it, and we didn’t do a thing.”
“Whether it’s politics or national complacency or stupidity, the fact is that we wasted two and half months,” said Haseltine.
Fauci, the director of National Institute of Allergy and Infectious Disease, acknowledged the mistake during a House Oversight Committee Hearing on Thursday: “It is a failing. I mean, let’s admit it."